ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP)
The ACSM Certified Clinical Exercise Physiologist (ACSM-CEP) examination is conducted by the American College of Sports Medicine. This examination gives you the best educational and practical experience standards in the health and fitness industry.CSM-CEPs make use of prescribed exercise, basic health behaviour interventions, and promote physical activity for individuals with chronic diseases or conditions; examples include, which is not limited to, individuals with cardiovascular, pulmonary, metabolic, orthopaedic, musculoskeletal, neuromuscular, neoplastic, immunologic and hematologic diseases. This provides primary and secondary prevention strategies designed to improve, maintain, or attenuate declines in fitness and health in populations ranging from children to older adults.
Exam Prerequisites
After successful becoming a certified Clinical Exercise Physiologist you will definitely achieve great heights in your career. However, you will require to have a few things as a prerequisites. These things are:
- Minimum of a bachelor’s degree in exercise science or equivalent and 1,200 hours of clinical hands-on experience
- A master’s degree in clinical exercise physiology and 600 hours of hands-on clinical experience.
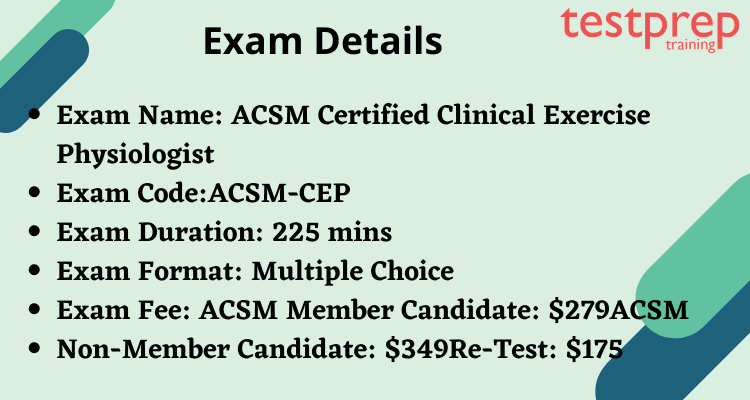
Exam Details
The ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP) examination consists of multiple-choice questions. The total time duration for this examination is 225 mins. This exam will cost you $279 if you are a member. However, if you are a non-member, the cost of the examination is $349. Also, if you want to reappear, in that case, the examination fee would be $175.
Exam Registration for ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP)
For registering yourself for the ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP) follow the following steps:
- Go to the Pearson VUE website.
- Choose your certification name
- Follow the prompt and complete the registration
- Make the payment and receive a confirmation for the examination.
For more information, visit ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP) FAQ.
Course Outline for ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP)
Domain I: Patient Assessment
A. Assess a patient’s medical record for information related to their visit.
- Knowledge of:
- the procedure to obtain the patient’s medical history through available documentation.
- the necessary medical records needed to properly assess a patient, given their diagnosis, and/or reason for referral.
- the procedure to obtain physician referral and medical records required for program participation.
- information and documentation required for program participation.
- the epidemiology, pathophysiology, progression, risk factors, key clinical findings, and treatments of chronic diseases.
- the techniques (e.g., lab results, diagnostic tests) used to diagnose chronic
- diseases, their indications, limitations, risks, normal and abnormal results.
- medical charting, terminology, and common acronyms.
- Skill in:
- interpreting information from medical records inpatient care and/or exercise prescription.
- assessing various vital signs.
- assessing participant physician referral and/or medical records to determine program participation status.
B. Interview patient regarding medical history for their visit and reconcile medications
- Knowledge of:
- establishment of rapport through health counseling techniques (e.g., the patientcentered approach), and nonjudgmental positive regard in creation of collaborative partnership.
- use of open-ended inquiry, active listening and attention to nonverbal behavior, interest and empathy.
- information and documentation required for program participation.
- the procedure to obtain informed consent from patient to meet legal requirements. commonly used medications in patients with chronic diseases, their mechanisms of action, and side effects. medical charting, terminology and common acronyms.
- Skill in:
- administering informed consent.
- interviewing patient for medical history pertinent to the reason for their visit and reconciling medications.
- active listening and usage of health counseling techniques.
- data collection during baseline intake assessment.
- proficiency in medical charting.
C. Obtain and assess resting biometric data (e.g., height, weight, ECG, arterial oxygen saturation, blood glucose, body composition, spirometry).
- Knowledge of:
- best practice-based intake assessment tools and techniques to assess and interpret clinical and health measures (e.g., height, weight, anthropometrics, body mass index, resting energy expenditure). medical therapies for chronic diseases and their effect on resting vital signs and symptoms.
- normal cardiovascular, pulmonary and metabolic anatomy and physiology.
- techniques for assessing signs and symptoms (e.g., peripheral pulses, blood pressure, edema, pain).
- 12-lead and telemetry ECG interpretation for normal sinus rate and rhythm or abnormalities (e.g., arrhythmias, blocks, ischemia,infarction).
- ECG changes associated with, but not limited to, drug therapy, electrolyte abnormalities, myocardial injury and infarction, congenital defects, pericarditis,pulmonary embolus and the clinical significance of each.
- Skill in:
- administering and interpreting resting biometric data to determine baseline health status.
- preparing a patient and ECG electrode application for resting ECGs
- assessing vital signs and symptoms at rest.
- assessing ankle brachial index using a hand-held Doppler
D. Determine a sufficient level of monitoring/supervision based on a preparticipation health screening.
- Knowledge of:
- normal physiologic responses to exercise.
- abnormal responses/signs/symptoms to exercise associated with different pathologies (e.g., cardiovascular, pulmonary, metabolic).
- pertinent areas of a patient’s medical history (e.g., any symptoms since their procedure, description of discomfort/pain, orthopedic issues).
- indications and contraindications to exercise testing and training.
- current published guidelines for treatment of cardiovascular, pulmonary and metabolic pathologies (e.g., American College of Cardiology/American Heart
- Association [ACC/AHA] Joint Guidelines, Global Initiative for Chronic Obstructive Lung Disease [GOLD], American Diabetes Association [ADA]).
- industry-recognized preparticipation health screening practices (e.g., the Physical Activity Readiness Questionnaire for Everyone [PAR-Q+], ACSM’s preparticipation screening algorithm).
- medical therapies for chronic diseases and their effect on the physiologic response to exercise.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise in patients with chronic diseases.
- abnormal signs and symptoms in apparently healthy individuals and those with chronic disease.
- methods used to obtain a referral for clinical exercise physiology services.
- Skill in:
- implementing industry-recognized preparticipation health screening practices.
- administering informed consent.
- selecting an exercise test based on a patient’s disease, condition and ability.
- determining risk and level of monitoring of patient using health history, medical history, medical records and additional diagnostic assessments.
- modifying exercise/physical activity program in response to medication use, timing and side effects.
E. Assess patient goals, needs, and objectives based on health and exercise history, motivation level, and physical activity readiness.
- Knowledge of:
- patient-centered health counseling techniques with nonjudgmental positive regard.
- assessment of patient goals and exercise history through use of open-ended inquiry, active listening and attention to nonverbal behavior and reflective listening.
- the effects of a sedentary lifestyle, including extended periods of physical inactivity and approaches to counteract these changes.
- behavior modification tools and techniques to assess patient’s expectations, goals and motivation level (e.g., health literacy, identification of real and perceived barriers, decisional balance).
- common barriers to exercise compliance and adherence (e.g., physical/disease state, environmental, demographic, vocation).
- known demographic factors related to likelihood of adherence and maintenance of exercise (e.g., age, gender, socioeconomic status, education, ethnicity).
- characteristics associated with poor adherence to healthy behaviors (e.g., low self-efficacy, poor social support
psychological issues associated with acute and chronic illness (e.g., anxiety, depression, social isolation, suicidal ideation).validated tools for measurement of psychosocial health status. - A variety of behavioral assessment tools (e.g., SF-36, health-related quality of life, Chronic Respiratory Disease Questionnaire) and strategies for their use.
- recognizing adverse effects of exercise in apparently healthy persons or those with chronic disease.
- Skill in:
- active listening and behavior modification techniques.
- counseling techniques and strategies to overcome real and perceived barriers.
- applying health behavior theories and strategies to strengthen patient barriers
- self-efficacy and optimize compliance and adherence in support of the achievement of a goal
- adapting/modifying an exercise program based on the unique needs of a patient
- administering commonly used screening tools to evaluate mental health status
Domain II: Exercise Testing
A. Select, administer, and interpret submaximal aerobic exercise tests (e.g., treadmill, step test, 6-minute walk).
- Knowledge of:
- tests to assess submaximal aerobic endurance
- the acute and chronic responses to aerobic exercise on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- the mechanisms underlying the acute and chronic responses to aerobic exercise on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- the effect of chronic diseases on acute and chronic responses to aerobic exercise.
- standard and/or disease-specific endpoints for submaximal aerobic exercise tests in apparently healthy individuals and those with chronic disease.
- typical submaximal aerobic test results and physiological values in trained and untrained individuals and those with and without chronic diseases.
- abnormal signs and symptoms in apparently healthy individuals and those with chronic disease.
- abnormal readings and results from exercise testing equipment (e.g., treadmill, ergometers, electrocardiograph, spirometer, metabolic cart, sphygmomanometer) that may indicate equipment malfunction.
- commonly used medications in patients with chronic diseases, their mechanisms of action, and side effects.
- Skill in:
- selecting the appropriate exercise test based on a patient’s disease, condition, and ability.
- administering and interpreting of submaximal aerobic exercise tests.
- modifying submaximal aerobic test and/or interpretation of results in response to medication use, timing, and side effects.
B. Select, administer, and interpret tests to assess musculoskeletal fitness, mobility, and balance.
- Knowledge of:
- tests to assess muscular strength, muscular endurance, flexibility and mobility.
- the acute and chronic responses to resistance exercise on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- tests to assess function and balance.
- the acute and chronic responses to flexibility and mobility exercise on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems.
- the mechanisms underlying the acute and chronic responses to resistance exercise on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- the effects of chronic diseases and their treatments on acute and chronic responses to resistance exercise, and an individual’s flexibility and mobility.
- standard and/or disease-specific endpoints for muscular strength, endurance, functional, and balance testing in apparently healthy individuals and those with chronic disease.
- typical muscular strength, muscular endurance, functional and balance test results, and physiological values in trained and untrained individuals and those with and without chronic diseases.
- commonly used medications in patients with chronic diseases, their mechanisms of action and side effects.
- Skill in:
- selecting the appropriate exercise test based on a patient’s disease, condition, and ability.
- administering and interpreting of submaximal aerobic exercise tests.
- modifying submaximal aerobic test and/or interpretation of results in response to medication use, timing, and side effects.
C. Select, prepare, and administer maximal, symptom-limited exercise tests.
- Knowledge of:
- contraindications to symptom-limited, maximal exercise testing, and factors associated with complications (e.g., probability of coronary heart disease, abnormal blood pressure).
- medical therapies for chronic diseases and their effect on the physiologic response to exercise.
- current practice guidelines/recommendations (e.g., AHA, Arthritis Foundation, National Multiple Sclerosis Society) for the prevention, evaluation, treatment, and management of chronic diseases.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise in patients with chronic diseases.
- cardiovascular, pulmonary, and metabolic pathologies, their clinical progression,
- diagnostic testing, and medical regimens/procedures to treat.
- normal and abnormal endpoints (i.e., signs/symptoms) for termination of exercise testing.
- abnormal signs and symptoms in apparently healthy individuals and those with chronic disease.
- medical therapies for chronic diseases and their effect on resting vital signs and symptoms.
- commonly used medications in patients with chronic diseases, their mechanisms of action and side effects.
- procedures to prepare a patient for ECG monitoring, including standard and modified lead placement.
- tools to guide exercise intensity (e.g., heart rate, perceived exertion, dyspnea scale, pain scale).
- the use of effective communication techniques (e.g., active listening and attention to nonverbal behavior, open-ended questioning, reflective listening skills) to address any concerns with the exam procedures.
- tests to assess maximal exercise tolerance.
- the physiologic responses during incremental exercise to maximal exertion in trained and untrained individuals and those with and without chronic diseases.
- standard and/or disease-specific endpoints for maximal exercise testing in apparently healthy individuals and those with chronic disease.
- typical maximal exercise test results and physiological values in trained and untrained individuals and those with and without chronic diseases.
- medical therapies for chronic diseases and their effect on clinical measurements and the physiologic response to maximal exercise.
- Skill in:
- administering a symptom-limited, maximal exercise test.
- preparing a patient for ECG monitoring during exercise.
- assessing vital signs and symptoms at rest and during exercise.
- interpreting ECG rhythms and 12-lead ECGs
D. Evaluate and report results from a symptom-limited maximal exercise test to medical providers and in the medical record as required.
- Knowledge of:
- the effects of chronic diseases on acute responses to maximal exercise.
- standard and/or disease-specific endpoints for maximal exercise testing in apparently healthy individuals and those with chronic disease.
- abnormal signs and symptoms in apparently healthy individuals and those with chronic disease during maximal exercise testing.
- typical maximal exercise test results and physiological values in trained and untrained individuals and those with and without chronic diseases.
- medical therapies for chronic diseases and their effect on clinical measurements and the physiologic response to maximal exercise.
- the interpretation of maximal exercise test measures (e.g., ECG response, oxygen saturation, rate-pressure product, claudication) and prognostic tools (e.g., Duke Treadmill Score) in context with the indication for the test, termination reason, and the patient’s medical history.
- Skill in:
- interpreting and reporting results from a symptom-limited, maximal exercise test.
- Synthesis
E. Identify relative and absolute contraindications for test termination and report to medical personnel as needed.
- Knowledge of:
- absolute contraindications and endpoints for terminating exercise testing.
- Skill in:
- interpreting and reporting results from a symptom-limited, maximal exercise test.
- assessing vital signs and symptoms at rest and during exercise.
- interpreting ECG rhythms and 12-lead ECGs.
Domain III: Exercise Prescription
A. Develop an individualized exercise prescription to support patient needs and goals for various exercise environments (e.g., home/community based, facility-based, virtual).
- Knowledge of:
- appropriate mode, volume, and intensity of exercise to produce favorable outcomes in apparently healthy individuals and those with chronic disease.
- the FITT-VP (frequency, intensity, time, type, volume, progression) principle for aerobic, muscular fitness/resistance training, and flexibility exercise prescription.
- the benefits and risks of aerobic, resistance, and flexibility exercise training in apparently healthy individuals and those with chronic disease.
- the effects of physical inactivity and methods to counteract these changes.
- normal and abnormal physiologic responses to exercise in healthy individuals and those with chronic diseases.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise training in patients with chronic diseases.
- disease-specific strategies or tools (e.g., breathing techniques, assistive devices, prophylactic nitroglycerin) to improve exercise tolerance in patients with chronic disease.
- appropriate modifications to the exercise prescription in response to environmental conditions in apparently healthy individuals and those with chronic disease.
- current practice guidelines/recommendations (e.g., U.S. Department of Health and Human Services, American College of Sports Medicine, Arthritis Foundation)
- for exercise prescription in apparently healthy individuals and those with chronic disease.
- applying metabolic calculations.
- a proper biomechanical technique for exercise (e.g., gait assessment, proper weight lifting form).
- muscle strength/endurance and flexibility modalities and their safe application and instruction.
- principals and application of exercise session organization.
- known demographic factors related to the likelihood of adherence and maintenance of exercise (e.g., age, gender, socioeconomic status, education, ethnicity, vocation).
- psychological issues associated with acute and chronic illness (e.g., anxiety, depression, social isolation, suicidal ideation).
- goal setting (e.g., SMART goals), reviewing, and constructive feedback in identifying barriers and reinforcing positive changes.
- risk factor reduction programs and alternative community resources (e.g., dietary counseling, weight management, smoking cessation, stress management, physical therapy/back care).
- incorporating health behavior theories into clinical practice.
- Skill in:
- interpreting functional and diagnostic exercise testing with applications to exercise prescription.
- interpreting muscular strength/endurance testing with applications to exercise prescription.
- developing an exercise prescription based on a participant’s clinical status and goals.
- applying metabolic calculations.
- applying strategies to reduce the risk of adverse events during exercise (e.g., gait belt, blood glucose monitoring).
- individualizing home exercise programs.
- optimizing patient compliance and adherence to exercise prescription
B. Communicate the exercise prescription, including the use of exercise equipment, and the importance of promptly reporting any adverse reactions or symptoms.
- Knowledge of:
- normal and abnormal physiologic responses to exercise in healthy individuals and those with chronic diseases.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise training in patients with chronic diseases and how to communicate this information with patients.
- lay terminology for an explanation of exercise prescription.
- the operation of various exercise equipment/modalities.
- a proper biomechanical technique for exercise (e.g., gait assessment, proper weightlifting form).
- muscle strength/endurance and flexibility modalities and their safe application and instruction.
- principals and application of exercise session organization.
- proper protocol to report adverse symptoms per facility policy.
- Skill in:
- communicating exercise prescription, exercise techniques, and organization of exercises
C. Explain and confirm patient understanding of exercise intensity and measures to assess exercise intensity (e.g., target heart rate, RPE, signs/symptoms, talk test).
- Knowledge of:
- tools to guide exercise intensity (e.g., heart rate, RPE, dyspnea scale, pain scale, talk test).
- abnormal signs and symptoms during exercise training in apparently healthy individuals and those with chronic disease.
- clear communication using patient learning style and/or health literacy to explain exercise intensity assessment.
- clear communication through effective communication techniques (e.g., active listening and attention to nonverbal behavior, open-ended questioning, reflective listening skills).
- Skill in:
- teaching methods used to guide exercise intensity.
D. Evaluate and modify the exercise prescription based on the patient’s compliance, signs/symptoms, and physiologic response to the exercise program, as needed.
- Knowledge of:
- physiologic effects due to changes in medical therapies for chronic diseases and their impact on exercise training.
- typical responses to aerobic, resistance and flexibility training in apparently healthy individuals and those with chronic disease.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise in patients with chronic diseases.
- disease-specific strategies or tools (e.g., breathing techniques, assistive devices, prophylactic nitroglycerin) to improve exercise tolerance in patients with chronic disease.
- abnormal signs and symptoms during exercise training in apparently healthy individuals and those with chronic disease.
- mode, volume and intensity of exercise to produce favorable outcomes in apparently healthy individuals and those with chronic disease.
- commonly used medications in patients with chronic diseases, their mechanisms of action, and side effects.
- modifications to the exercise prescription in response to environmental conditions in apparently healthy individuals and those with chronic disease.
- systems for tracking participant progress in both preventive and rehabilitative exercise programs.
- participant progress in a preventive and rehabilitative exercise program given gender, age, clinical status, pre-program fitness level, specifics of the exercise program (e.g., walking only vs. comprehensive monitored program), and rate of program participation.
- Skill in:
- helping patients identify barriers and providing strategies to overcome them.
- assessing the adequacy of patient’s progress in a preventive or rehabilitative exercise program given age, sex, gender, clinical status, specifics of the exercise program, and rate of program participation.
- developing an individualized exercise prescription.
- using patient feedback and developing individualized exercise prescription and/or care plan.
- active listening.
- modifying an exercise prescription specifically to meet a patient’s individual needs and goals.
Domain IV: Exercise Training and Leadership
A. Discuss and explain exercise training plan, patient, and clinician expectations and goals.
- Knowledge of:
- health counseling techniques (e.g., the patient-centered approach) and nonjudgmental positive regard in the creation of the collaborative partnership.
- effective communication techniques, while using clear, patient-friendly terms (e.g., active listening, body language, motivational interviewing).
- factors related to health literacy skills and capacity.
- cardiovascular, pulmonary, and metabolic pathologies, their clinical progression,
- diagnostic testing and medical regimens/procedures to treat.
- the FITT-VP principle (frequency, intensity, time, type, volume, progression) for aerobic, muscular fitness/resistance training, and flexibility exercise prescription.
- the timing of daily activities (e.g., medications, dialysis, meals, glucose monitoring) and their effect on exercise training in patients with chronic diseases.
- disease-specific strategies or tools (e.g., breathing techniques, assistive devices,
- prophylactic nitroglycerin) to improve exercise tolerance in patients with chronic disease.
- exercise training concepts specific to industrial or occupational rehabilitation, such as work hardening, work conditioning, work fitness, and job coaching.
- commonly used medication for cardiovascular, pulmonary, and metabolic diseases.
- Skill in:
- identifying the unique needs of those with chronic diseases in exercise prescription.
- communicating the exercise prescription and related exercise programming techniques.
- educating patients following the observation of problems with comprehension and performance of their exercise program.
- applying techniques to reduce risks of adverse events during exercise (e.g., gait belt, blood glucose monitoring).
- educating participants on the use and effects of medications.
- communicating with participants from a wide variety of educational backgrounds.
- using patient feedback to develop individualized exercise prescription and/or care plan.
- active listening
B. Identify, adapt and instruct in cardiorespiratory fitness, muscular strength, and endurance, flexibility, coordination, and agility exercise modes.
- Knowledge of:
- the selection, operation, and modification of exercise equipment/modalities based on the disease, condition, and ability of the individual.
- a proper biomechanical technique for exercise (e.g., gait, weight lifting form).
- exercise techniques to reduce risk and maximize the development of cardiorespiratory fitness, muscular strength, and flexibility.
- mode, volume, and intensity of exercise to produce favorable outcomes in apparently healthy individuals and those with chronic disease.
- disease-specific strategies or tools (e.g., breathing techniques, assistive devices, prophylactic nitroglycerin) to improve exercise tolerance in patients with chronic disease.
- counseling techniques to optimize participant’s disease management, risk reduction, and goal attainment.
- modifications to the exercise prescription in response to environmental conditions in apparently healthy individuals and those with chronic disease.
- the benefits and risks of aerobic, resistance, and flexibility training in apparently healthy individuals and those with chronic diseases.
- Skill in:
- identifying unique needs and goals of a patient and adapting/modifying an exercise program.
- supervising and leading patients during exercise training.
- communicating the exercise prescription and related exercise programming techniques.
- educating patients following the observation of problems with comprehension and performance of their exercise program.
C. As indicated, provide patient monitoring (e.g., pulse oximetry, biometric data) and supervision during exercise.
- Knowledge of:
- normal and abnormal exercise responses, signs and symptoms associated with different pathologies (i.e., cardiovascular, pulmonary, metabolic,
- orthopedic/musculoskeletal, neuromuscular, neoplastic, immunologic, and hematologic disorders).
- normal and abnormal 12-lead and telemetry ECG interpretation.
- exercise program monitoring (e.g., telemetry, oximetry, glucometer).
- disease-specific strategies or tools (e.g., breathing techniques, assistive devices, prophylactic nitroglycerin) to improve exercise tolerance in patients with chronic disease.
- the benefits and risks of aerobic, resistance, and flexibility training in apparently healthy individuals and those with chronic disease.
- the components of a patient’s medical history necessary to screen during program participation.
- commonly used medications in patients with chronic diseases, their mechanisms of action, and side effects.
- the timing of daily activities with exercise (e.g., medications, meals, insulin/glucose monitoring).
- how medications or missed dose(s) of medications impact exercise and its progression.
- psychological issues associated with acute and chronic illness (e.g., depression, social isolation, suicidal ideation).
- health counseling techniques and nonjudgmental positive regard.
- Skill in:
- monitoring and supervising patients during exercise training.
- interpreting ECG rhythms and 12-lead ECGs.
- recognizing the adverse effects of exercise in apparently healthy persons or those with pathologies of acute and/or chronic disease.
- applying and interpreting tools for clinical assessment (e.g., telemetry, oximetry, and glucometer, perceived rating scales).
- modifying exercise/physical activity programming in response to medication use, timing and side effects.
D. Evaluate the patient’s contraindications to exercise training and associated risk/benefit and modify the exercise/activity program accordingly.
- Knowledge of:
- the contraindications to exercise training and factors associated with complications in apparently healthy individuals and those with chronic disease.
- the benefits and risks of aerobic, resistance and flexibility training in apparently healthy individuals and those with chronic disease.
- abnormal signs and symptoms in apparently healthy individuals and those with chronic disease.
- the acute and chronic responses to exercise training on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- cardiovascular, pulmonary, and metabolic pathologies, diagnostic testing and
- medical management regimens and procedures.
- Skill in:
- identifying contraindications to exercise training.
- modifying the exercise program based on participant’s signs and symptoms, feedback, and exercise responses.
E. Evaluate, document, and report the patient’s clinical status and response to exercise training in medical records.
- Knowledge of:
- the techniques (e.g., lab results, diagnostic tests) used to diagnose different pathologies, their indications, limitations, risks, normal and abnormal results.
- the acute and chronic responses to exercise training on the function of the cardiovascular, respiratory, musculoskeletal, neuromuscular, metabolic, endocrine, and immune systems in trained and untrained individuals.
- normal and abnormal exercise responses, signs, and symptoms associated with different pathologies (i.e., cardiovascular, pulmonary, metabolic, orthopedic/musculoskeletal, neuromuscular, neoplastic, immunologic, and hematologic disorders).
- how chronic diseases may affect the acute and chronic responses exercise training.
- abnormal signs or symptoms which may be associated with worsening of chronic disease.
- proper medical documentation according to generally accepted principles and individual facility standards.
- regulations relative to documentation and protecting patient privacy (e.g., written and electronic medical records, Health Insurance Portability and Accountability Act [HIPAA]).
- Skill in:
- summarizing patient’s exercise sessions, outcomes and clinical status into patient’s medical record.
- proficiency in medical charting.
F. Discuss clinical status and response to exercise training with patients and adapt and/or modify the exercise program, as indicated.
- Knowledge of:
- common barriers to exercise compliance and adherence (e.g., physical, environmental, demographic).
- effective communication techniques (e.g., active listening, body language).
- techniques to adapt/modify exercise program based on a patient’s needs.
- assess patient’s individual progress based on known cardiorespiratory fitness, muscular strength, and flexibility improvements expected within a given population.
- assess the patient’s tolerance to exercise modality and suggest comparable alternative modalities.
- Skill in:
- communicating health information based on a patient’s learning style and health literacy.
- modifying the exercise program based on participant’s signs and symptoms, feedback and exercise responses.
- summarizing patient’s exercise sessions, outcomes and clinical status into patient’s medical record.
- Application
G. Promptly report new or worsening symptoms and adverse events in the patient’s medical record and consult with the responsible health care provider.
- Knowledge of:
- proper medical documentation according to generally accepted principles and individual facility standards.
- the scope of practice of health care professionals (e.g., physical therapist, nurse, dietician, psychologist).
- abnormal signs and symptoms during exercise training in apparently healthy individuals and those with chronic disease.
- the effects of chronic diseases on the acute and chronic responses to exercise training.
- Skill in:
- assessing normal and abnormal responses to exercise.
- educating patients following the observation of problems with comprehension and performance of their exercise program.
- evaluating and prompt reporting of a patient’s adverse response to an exercise program in accordance with facility policy and procedures.
Domain V: Education and Behavior Change
A. Continually evaluate patients using observation, interaction, and industry-accepted tools, to identify those who may benefit from counseling or other mental health services using industry-accepted screening tools.
- Knowledge of:
- establishment of rapport through use of open-ended questions, active listening and attention to nonverbal behavior, interest and empathy.
- the psychological issues associated with acute and chronic illness (e.g., anxiety, depression, social isolation, hostility, aggression, suicidal ideation).
- theories of health behavior change (e.g., Social Cognitive Theory [SCT], Health Belief Model [HBM], Transtheoretical Model [TTM])).
- industry accepted screening tools to evaluate mental health status (e.g., SF-36, Beck Depression Index).
- signs and symptoms of failure to cope during personal crises (e.g., job loss, bereavement, illness).
- accepted methods of referral to behavioral health or other specialists as needed.
- Skill in:
- administering commonly used screening tools to evaluate mental health status.
- applying and interpreting psychosocial assessment tools.
- identifying patients who may benefit from behavioral health services.
B. Assess patient’s understanding of their disease and/or disability and conduct education to teach the role of lifestyle in the prevention, management, and treatment of the disease.
- Knowledge of:
- active listening, open-ended questioning, reflective listening skills.
- patient-centered health counseling techniques (e.g., Five-A’s Model, MotivationalInterviewing). factors related to health literacy skills and capacity.
- barriers to exercise compliance (e.g., physical/disease state, psychological environmental, demographic).
- social-ecological model.
- psychological issues associated with acute and chronic illness (e.g., anxiety, depression, suicidal ideation).
- theories of health behavior change (e.g., Social Cognitive Theory, Health BeliefModel, Transtheoretical Model).
- tools to determine a patient’s knowledge and their readiness to change (e.g., scoring rulers, decisional balance).
- the benefits and risks of aerobic, resistance, flexibility, and balance training in apparently healthy individuals and those with chronic disease.
- the health benefits of a physically active lifestyle, the hazards of sedentary behavior, and current recommendations from U.S. national reports on physical activity (e.g., U.S. Surgeon General, National Academy of Medicine).
- abnormal signs and symptoms during rest and exercise in apparently healthy individuals and those with chronic disease.
- the epidemiology, pathophysiology, progression, risk factors, key clinical findings, and treatments of chronic disease.
- education content and program development based on participant’s medical history, needs and goals.
- medical therapies and commonly used medications for chronic diseases and their effect on resting vital signs, clinical measurements, and the response to exercise.
- disease-specific strategies and tools to improve exercise tolerance (e.g., breathing techniques, insulin pump use, prophylactic nitroglycerin).
C. Apply health behavior change techniques (e.g., Motivational Interviewing, Cognitive Behavioral Therapy [CBT], Health Coaching) based upon assessment of readiness to change according to Transtheoretical Model (TTM)
- Knowledge of:
- active listening, open-ended questioning, reflective listening skills.
- barriers to exercise compliance and adherence (e.g., physical/disease state, psychological environmental, demographic, vocational).
- known demographic factors related to likelihood of adherence and maintenance of exercise (e.g., age, gender, socioeconomic status, education, ethnicity).
- characteristics associated with poor adherence to healthy behaviors.
- health counseling techniques (e.g., the patient-centered approach).
- goal setting (e.g., SMART goals), reviewing, and constructive feedback in support of patient for best likelihood of achievement of goals.
- theories of health behavior change (e.g., Social Cognitive Theory [SCT], Health Belief Model [HBM], Transtheoretical Model ([TTM]).)
- application of behavior-change techniques (e.g., motivational interviewing, cognitive-behavioral therapy, health coaching).
- eliciting change talk by patient through motivational interviewing technique.
- development of self-efficacy (task and barriers) in exercise behaviors.
- Skill in:
- effective use of behavior-change techniques.
- active listening of patient feedback and consideration with decision making of exercise prescription and/or care plan.
- promoting patient engagement in process of fitness and health improvement.
- creating clear communication using medical terminology suitable for patient’s health literacy and/or learning style.
D. Promote adherence to healthy behaviors through a patient centered approach (e.g., addressing barriers, engaging in active listening, expressing interest and empathy,increasing self-efficacy, teaching relapse prevention techniques and identifying support).
- Knowledge of:
- establishment of rapport through use of open-ended questions, active listening and attention to nonverbal behavior, interest and empathy.
- health counseling techniques (e.g., the patient-centered approach) and nonjudgmental positive regard in creation of collaborative partnership.
- theories of health behavior change (e.g., Social Cognitive Theory [SCT], Health Belief Model [HBM], Transtheoretical Model [TTM]barriers to exercise compliance and adherence (e.g., physical/disease state, psychological environmental, demographic, vocational).
- known demographic factors related to likelihood of adherence and maintenance of exercise (e.g., age, sex, gender, socioeconomic status, education, ethnicity).
- tools for measuring clinical exercise tolerance (e.g., heart rate, glucometry, subjective rating scales), and consideration of affect regulation in determining exercise prescription.
- risk factor reduction programs and alternative community resources (e.g., wellness coaching, smoking cessation, physical therapy/back care, dietary counseling).
- goal setting (i.e., SMART goals), reviewing, and constructive feedback in support of patient for best likelihood of achievement of goals.
- eliciting change talk by patient through motivational interviewing technique.
- development of self-efficacy (task and barriers) in exercise behaviors.
- promotion of patient intrinsic motivation (e.g., supporting feelings of autonomy and competence, positive feedback, enjoyment) in facilitating long-term adherence to exercise.
- community resources (exercise and/or health support) available for participant
- use following program conclusion and/or discharge.
- relapse prevention techniques (e.g., proactive problem solving, managing lapses, maintaining high self-efficacy in health behaviors, identifying social support).
- guidance of social support (e.g., reassurance, nurturance, supportive exercise groups).
- Skill in:
- effective use of behavior-change techniques.
- active listening and receptiveness to patient feedback in decision making of exercise prescription and/or care plan.
- effective communication with participants from a wide variety of backgrounds.
- promoting patient engagement in process of fitness and health improvement.
Domain VI: Legal and Professional Responsibilities
A. Evaluate the exercise environment and perform regular inspections of any emergency equipment and practice emergency procedures (e.g., crash cart, activation of emergency procedures) per industry and regulatory standards and facility guidelines.
- Knowledge of:
- government and industry standards and guidelines (e.g., American Association of Cardiovascular and Pulmonary Rehabilitation [AACVPR], American College of Sports Medicine [ACSM], Academy of Nutrition and Dietetics, Health Insurance Portability and Accountability Act [HIPAA], Joint Commission: Accreditation, Health Care, Certification [JCAHO], Occupational Health and Safety Act [OHSA], Americans with Disabilities Act, American Diabetes Association [ADA]).
- the operation and routine maintenance of exercise equipment.
- current practice guidelines/recommendations for facility layout and design.
- standards of practice during emergency situations (e.g., American Heart Association, American Red Cross).
- local and institutional procedures for activation of the emergency medical system.
- standards for inspection of emergency medical equipment.
- risk-reduction strategies, universal precautions, basic life support, emergency equipment, and standard emergency procedures.
- Skill in:
- adhering to legal guidelines and documents
- implementing facility safety policies and procedures.
- applying basic life support procedures (e.g., Cardiopulmonary resuscitation [CPR], automated external defibrillator [AED]).
- the use of medical terminology.
B. Follow industry-accepted scopes of practice, ethical, legal (e.g., data privacy, informed consent), and business standards.
- Knowledge of:
- professional liability and common types of negligence seen in exercise rehabilitation and exercise testing environments.
- the legal implications of documented safety procedures, the use of incident documents, and ongoing safety training.
- the scope of practice of healthcare professionals (e.g., physical therapist, nurse, dietician, psychologist).
- current practice guidelines/recommendations (e.g., National Heart, Lung, and Blood Institute, Arthritis Foundation, National Multiple Sclerosis Society) for the prevention, evaluation, treatment, and management of chronic diseases.
- regulations relative to documentation and protecting patient privacy (e.g., written and electronic medical records, Health Insurance Portability and Accountability Act [HIPAA]).
- Skill in:
- proficiency in medical charting.
- applying industry and regulatory standards.
- adhering to legal guidelines and documents.
- the use of medical terminology.
Preparatory Guide for ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP)
After getting all the details of the examination. It is time to start preparing for it. We are sharing a preparatory guide specially designed for ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP) examination by our experts.
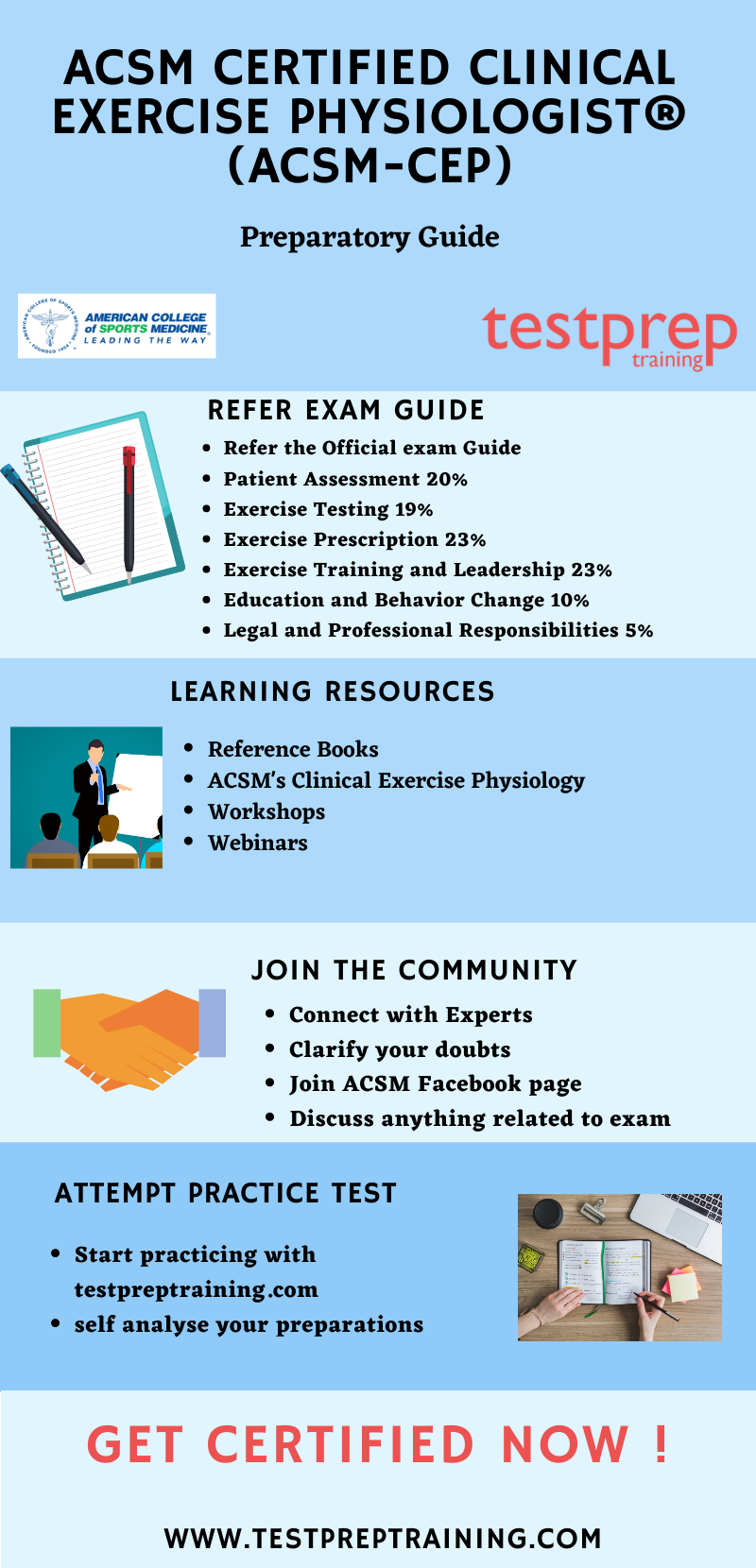
Refer the Exam Guide
The course domains and modules act as a blueprint for the exam. Therefore you must refer the ACSM Certified Clinical Exercise Physiologist® (ACSM-CEP) before commencing its preparations to excel in the exam. Also, exam objectives are very important when it comes to preparing the exam strategy. Here, we have provided you with the exam objectives.
- Patient Assessment 20%
- Exercise Testing 19%
- Exercises Prescription 23%
- Exercise Training and Leadership 23%
- Education and Behavior Change 10%
- Legal and Professional Responsibilities 5%
Learning Resources
The second step to successfully clear any examination is to practice from the resources. ACSM provides you with workshops and webinars where you can learn about the ACSM Certified Clinical Exercise Physiologist (ACSM-CEP) examination.
Reference Books
It is very important to study from the right book. There are ample number of books available in the market for this examination. You can also refer to the official book shared by ACSM. This book will help you in preparing for the examination:
- ACSM’s Clinical Exercise Physiology: This book offers research-based coverage of more than 35 conditions commonly seen in practice—from a host of cardiovascular disorders to immunological/hematological disorders.
Join Study Groups
It is very important to interact with people who have a common aim in life. Joining study groups is a good way to get yourself fully involved with the certification exam you applied for. These groups will help you get up to date with the latest changes or any update happening exam. Also, these groups contain both beginners as well as professionals. You can also join the ACSM Facebook Study Group page where you participate in Live chats and discussions.
Practice with testpreptraining
It is very important to practice what you have learned so that you are in a position to analyze your practice, by practicing you will be able to improve your answering skills that will result in saving a lot of time. Moreover, the best way to start doing practice tests is after completing one full topic as this will work as a revision part for you. Start practicing now!